This page explains what insulin sensitivity is and what factors affect it. When the body is more sensitive to insulin, it needs a smaller dose to lower blood sugar and keep it within a healthy range. Controlling diabetes is much easier if you can get by with low doses of insulin or even no daily injections at all.
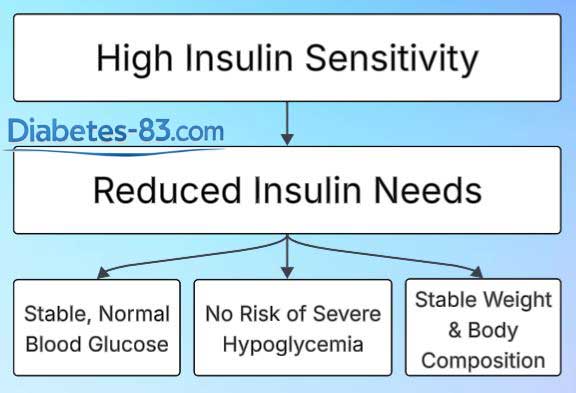
Besides lowering blood sugar, insulin also promotes fat storage and weight gain. High doses can lead to increased obesity, which is especially harmful in diabetes. That’s why maintaining good insulin sensitivity is important. It allows the body to function with lower insulin doses or sometimes even without daily shots.
By the end of this page, you will be able to:
- Understand why your insulin needs often rise or fall
- Create a clear, practical plan to improve your insulin sensitivity and maintain it high
- Manage your diabetes with greater confidence
- Gain a deeper understanding than most board-certified endocrinologists and diabetes educators
Unfortunately, insulin injections often work in unstable and unpredictable ways. This issue remains a major challenge in diabetes treatment. I do not expect it to be solved anytime soon. Still, the effects of insulin shots are not entirely random. People with diabetes can, to a great extent, predict how much a given dose will lower their blood sugar and how quickly it will happen.
With time and experience, anyone with diabetes can learn to estimate the appropriate insulin doses that work OK for them. To achieve that, you should understand the factors that affect insulin sensitivity. That’s exactly what this page will help you learn.
The Dangers of Low Insulin Sensitivity
Low insulin sensitivity, also called insulin resistance, is a metabolic disorder where the body responds poorly to insulin. People with diabetes who have insulin resistance need high doses of insulin to bring their blood sugar down. For them, small doses are ineffective.
Insulin doesn’t just lower blood glucose; it also encourages the body to store fat. The more fat the body stores, the less sensitive it becomes to insulin. In short, obesity makes insulin resistance worse.
Let’s say a person’s insulin sensitivity drops—for example, due to reduced physical activity. As a result, they need higher doses of insulin. However, higher insulin doses can lead to more fat storage. In turn, the extra fat further reduces insulin sensitivity. It forces insulin doses to increase again. It leads to even more weight gain. This situation is known as a vicious circle.
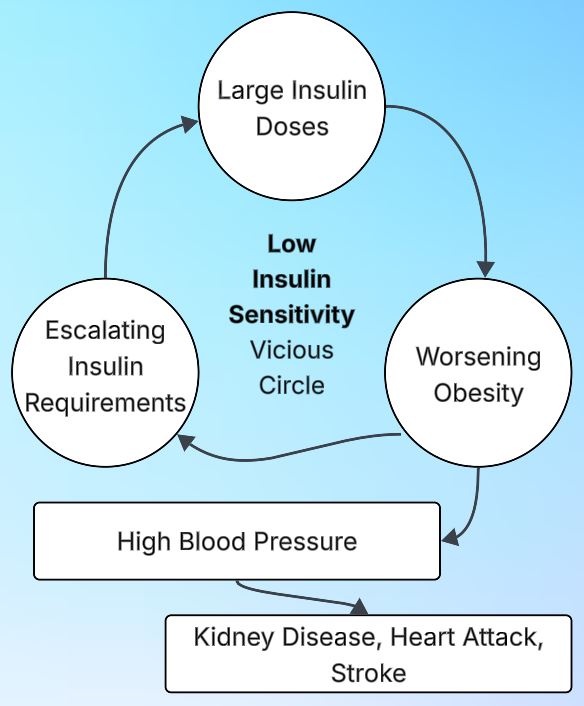
This vicious circle is prevalent. It affects millions of people with type 2 diabetes and many with type 1 diabetes as well. They often face a series of connected problems:
- They can’t lose weight because they’re using high doses of insulin.
- Since they can’t lose weight, their insulin sensitivity stays low, so they continue needing high doses.
- These high doses increase the risk of severe hypoglycemia, which can sometimes be fatal.
- Excess body fat raises blood pressure.
- Their hypertension often doesn’t respond well to medication.
- Poorly controlled diabetes and high blood pressure can lead to early death from heart attack, stroke, or kidney failure.
Escaping this cycle isn’t easy. Losing weight is a difficult task on its own—and nearly impossible while taking high doses of insulin. However, with enough motivation, switching to a low-carbohydrate approach to diabetes management can help break the cycle.
Your insulin sensitivity is, to a great extent, within your control. Below, you’ll learn how to improve and keep it high over time. Many factors affect insulin sensitivity. I’ll explain each of them in detail and, more importantly, show you how to influence them in a way that works in your favor.
Key Factors That Influence Insulin Sensitivity
Insulin sensitivity depends primarily on your lifestyle. Heredity and external factors also play a role. Here are the key factors, listed from most to least important:
- Nutrition, diet
- Body fat percentage and fat-to-muscle ratio
- Current blood glucose levels
- Physical activity
- Use of certain medications
- Viral and bacterial infections
- Hormonal balance: thyroid, cortisol, and other hormones
- Genetic predisposition to insulin resistance
- Age
- Time of day
- For women, the stage of the menstrual cycle
- Weather and air temperature
- Place and depth of insulin injection
- Alcohol consumption
Below, you’ll find detailed explanations of every factor and practical advice on influencing them.
Nutrition, Diet
Nutrition is the single most significant factor in managing diabetes. For people with diabetes who are motivated to stay healthy and avoid complications, a low-carbohydrate diet is essential. A standard “balanced” diet and a vegetarian approach are incompatible with fine blood sugar control. Low-carb eating is the most effective way to improve insulin sensitivity and maintain stable glucose levels.
A diet high in carbohydrates forces the body to rely on large doses of insulin. In type 2 diabetes, patients often take harmful medications that push the pancreas to produce more insulin. Both high-dose insulin injections and these medications can drive people into the vicious cycle described earlier. It often results in disability and early death.
Carbohydrates are tasty—but are they worth risking your life for? For most people, the answer is no. Instead of turning to high-carb foods for comfort or pleasure, try finding other sources of enjoyment and satisfaction that support your health. Check the page with the lists of recommended and restricted foods to learn how to enjoy life while avoiding harmful food choices.
Family members of people with diabetes also benefit from switching to a low-carb diet alongside their loved ones. Over time, they notice the following surprising advantages:
- They age more slowly than their peers
- Their vision stays sharper with age
- They spend significantly less on dental care
Making these dietary changes together can improve everyone’s health—not just the person with diabetes.
Body Fat Percentage
Obesity significantly reduces insulin sensitivity. So, one of the most effective ways to improve it is to lose excess weight. Of course, this is easier said than done. Most popular weight-loss methods—like fad diets or prolonged fasting—don’t work well in the long run. And the ones that do often come with serious side effects, such as muscle loss or depression.
If you cannot lose excess fat, you can still work to offset its harmful effects. The goal is to boost your insulin sensitivity and keep it high by focusing on other controllable factors. The two most effective strategies are following a low-carbohydrate diet and staying physically active.
Sometimes, I meet people who look slim but have low muscle mass and high body fat. Fat has quietly replaced much of their muscle tissue. Despite their appearance, they struggle with low insulin sensitivity—just like people with visible obesity. The good news is that the same strategies can help them: improving diet, increasing physical activity, and building muscle.
Blood Glucose Level
When blood glucose levels are very high, insulin sensitivity drops sharply. This effect is significant for people with diabetes, so this factor appears near the top of our list.
Let’s look at the explanatory example. Suppose your current blood glucose is 145 mg/dL. Based on your experience, 1 unit of rapid-acting insulin typically brings it down to about 100 mg/dL. In other words, 1 unit lowers your blood sugar by roughly 45 mg/dL.
Next, consider when your blood glucose is much higher, say, 280 mg/dL. To bring it down to 100 mg/dL, you’d need to lower it by 180 mg/dL. If you divide 180 by 45, you get a calculated dose of 4 units of insulin. But here’s the catch: that dose often isn’t enough. When blood glucose is very high, insulin sensitivity drops, and the usual dose becomes ineffective. You might need two to three times more insulin than the above calculation suggests.
Bringing very high blood sugar back to normal usually requires injecting a large insulin dose. Also, drink some water, as high blood sugar often causes dehydration. Rehydrating helps your body respond better to insulin shots and can support faster recovery.
High doses of insulin come with several drawbacks:
- Increased risk of severe hypoglycemia
- Faster depletion of your insulin supply
- Long-term metabolic harm—insulin encourages the body to store fat rather than burn it
The key takeaway is that it is much better to prevent your blood sugar from rising too high in the first place. Acting early requires much smaller insulin doses. They are usually two to three times less than what is needed to correct a significant spike later on.
Learn here how to monitor your blood glucose levels properly to avoid big spikes. Find out why using a continuous glucose monitoring system is highly recommended.
In the example above, we didn’t account for food that may still be digesting in the diabetic’s body. It refers to food that hasn’t yet raised blood sugar but will do so over time. In real life, you should always try to consider such delayed effects when calculating insulin doses. However, the purpose of the simplified example was to highlight just one point: how insulin sensitivity decreases when blood glucose levels are very high.
Important Warning:
For your insulin dose calculation, do not rely on the example value of 1 unit of ultra-short-acting insulin lowering blood sugar by 45 mg/dL. This number is only an illustration—it varies greatly from person to person and must be determined individually.
Using a general estimate from Wikipedia, a health ministry website or any other source can be dangerous. Doing so puts you at serious risk of severe hypoglycemia. Always base your insulin dosing on your individualized data and guidance from a qualified healthcare provider.
Physical Activity
Physical activity improves insulin sensitivity for several key reasons:
- It helps burn stored glucose (glycogen) from the liver and muscles
- It promotes muscle growth and improves the muscle-to-fat ratio in the body
These effects make your body more responsive to insulin immediately after exercise and in the long term.
As insulin sensitivity increases with physical activity, people with type 1 diabetes are at higher risk of hypoglycemia during and after exercise. To stay safe, check your blood sugar every 15 minutes while exercising. Keep glucose tablets or liquid solution within reach in case your levels drop too low.
You’ll need to determine how much physical activity affects your insulin sensitivity. This response is highly individual and can vary significantly from person to person. With consistent observation over days and weeks, you’ll gradually learn how to adjust your insulin doses based on your planned exercise routine. Avoid relying on generic formulas or preset adjustment factors—even if you find them online. They may not apply to your body and could lead to wrong results.
Physical activity ranks second only to a low-carb diet in promoting longevity. It helps to prevent chronic diabetes complications and common age-related diseases. Exercise isn’t just essential for people with diabetes—it’s vital for anyone who wants to stay fit and healthy throughout their life. Include cardiovascular workouts and strength training in your routine for the best results.
Medications That Affect Insulin Sensitivity
Many commonly used medications can harm your metabolism in different ways—one of the most crucial being a reduction in insulin sensitivity. You’ll find more details about it below. It’s wise to spend some time researching the potential benefits and risks of the drugs. Before starting any new medication, consult your doctor.
It’s no surprise that many people look for—and are willing to pay for—pills to help fight insulin resistance. Hundreds of millions hope to replace healthy eating and physical activity with medication. To some extent, metformin makes this possible. This drug has been used for half a century already. It has a strong track record of safety and effectiveness.
However, if your goal is to live a long, healthy life and avoid disability, you need to do two key things:
- Follow a low-carb diet
- Stay physically active
Metformin can be a helpful addition—but it should not replace these core lifestyle interventions.
There are several medications beyond metformin claiming to improve insulin sensitivity. I talk about them in more detail below. They all come with serious side effects. It’s best to approach them with caution. There are no miracle drugs. Lasting improvements come from lifestyle changes, not shortcuts.
Food Supplements
Many people take dietary supplements hoping to improve insulin sensitivity. Common examples include:
- Omega-3 fatty acids
- Chromium (picolinate or polynicotinate)
- Berberine
However, these supplements are unlikely to have any meaningful effect on insulin resistance. You shouldn’t expect them to replace the proven benefits of a proper diet and regular physical activity.
Diabetes Pills
To improve your insulin sensitivity, consider taking metformin alongside a low-carb diet. This combination is generally safe and well-supported by the accumulated practical experience. Before starting metformin, get blood and urine tests to check your kidney function. It ensures the medication is safe for you. Metformin may harm people with advanced kidney disease.
Another class of diabetes medications worth mentioning is thiazolidinediones, which includes:
- Rosiglitazone
- Pioglitazone
Like metformin, these drugs enhance insulin sensitivity. However, unlike metformin, they have been linked to serious side effects. Because of these risks, thiazolidinediones have fallen out of favor in recent years. Most doctors now prescribe them rarely—and for good reason.
Most other diabetes medications don’t increase insulin sensitivity directly. However, they can improve it indirectly by helping to lower blood sugar through different mechanisms. For example:
- GLP-1 receptor agonists reduce appetite, which can lead to weight loss.
- SGLT2 inhibitors (sodium-glucose cotransporter inhibitors) help the kidneys remove excess glucose through urine, lowering blood sugar levels. Find out more about them here.
These effects may support better insulin sensitivity over time. Please note that all drugs belonging to the listed groups are not a panacea and have serious side effects.
Another popular class of diabetes medications is the sulfonylureas. This group includes glibenclamide (Glyburide), glipizide (Glucotrol, Minodiab), gliclazide (Diamicron, Diaprel), and glimepiride (Amaryl). Learn more about these prevalent drugs here.
Glucocorticoids
Glucocorticoids—such as prednisolone, dexamethasone, and similar drugs—are among the most harmful medications when it comes to insulin sensitivity. They severely disrupt metabolism and can cause insulin requirements to rise dramatically. What makes them particularly destructive is the long-lasting impact. Even after stopping these drugs, their crushing effects on insulin sensitivity can persist for years—and sometimes for life.
Glucocorticoids promote weight gain and worsen diabetes. They can even cause diabetes in people who didn’t have it before—a condition known as glucocorticoid-induced diabetes, which is a recognized medical diagnosis. At the same time, these drugs suppress the immune system. This immune system suppression is usually why doctors prescribe them.
Unfortunately, in many situations, glucocorticoids are unavoidable. They are often the only life-saving treatment for patients facing severe autoimmune or inflammatory diseases. While their use carries serious long-term side effects, including worsening insulin sensitivity, doctors justify it because they save lives in critical moments.
If you need to take glucocorticoids for a chronic condition, ask your doctor about alternative treatments. Be persistent about it. One option to explore is the Carnivore Diet, which some people use to manage autoimmune and inflammatory diseases. You can read more about it here.
Depression Pills
Most sources say that SSRIs and other antidepressants can either decrease or increase insulin sensitivity. However, I remain skeptical about the research supporting their effectiveness.
With a bit of research, you can find many compelling reasons to avoid antidepressants. This caution applies even to patients with severe depression and, undoubtedly, to everyone else. For a critical perspective, consider reading the works of Peter C. Gøtzsche.
Consider cognitive behavioral therapy (CBT) as an effective treatment for depression. Today, many smartphone chatbots can serve as free, accessible “pocket psychotherapists.” You can also learn how to manage your blood sugar well here. Mastering this skill builds self-confidence and can help combat depression. Use these tools and try to avoid relying on medications whenever possible.
Cholesterol Medications
Statins are the most commonly prescribed cholesterol-lowering drugs. However, many statins can reduce insulin sensitivity and worsen blood sugar control in people with diabetes. They also carry a range of other serious side effects. Some experts believe that organized medicine tends to overstate the benefits of statins while downplaying their risks.
Official medicine claims that statins have only a moderate negative effect on diabetes. Medical journal articles often state that these drugs raise glycated hemoglobin (HbA1c) by no more than 1.0–1.5%. I wouldn’t call it a moderate effect. You can learn more about normal blood glucose and HbA1c levels here.
If you spend just half an hour researching, you’ll find many strong arguments for avoiding statins. You should never take these drugs, no matter how high your cholesterol is. I recommend starting your research with Dr. Malcolm Kendrick’s blog.
Some supplement enthusiasts take gigantic doses of vitamin B3 (niacin)—1 to 3 grams daily—to lower cholesterol. It is a bad idea. Don’t do it! At these high doses, niacin lowers insulin sensitivity and raises blood sugar in people with diabetes. Other common side effects include facial redness and itching, nausea, vomiting, diarrhea, and damage to the liver, heart, and eyes.
I strongly doubt that lowering your cholesterol with medication or supplements will extend your life. It may do the opposite. Remember, cholesterol is not a poison — it’s a vital substance for your body. Unlike high blood sugar, seeing elevated cholesterol in your blood tests, including LDL, is good news.
High Blood Pressure Pills
Two well-known older blood pressure medications—hydrochlorothiazide and propranolol—can significantly worsen insulin sensitivity when taken daily. These pills were once very popular but have since fallen out of favor. Most doctors know about their crippling effects on metabolism and usually avoid prescribing them. Additionally, these are old, cheap drugs, so pharmaceutical companies don’t offer kickbacks for prescribing them.
Official medicine claims that many modern hypertension drugs improve insulin sensitivity. However, this effect is very weak—almost negligible. In practice, I would say it’s barely noticeable.
After switching to a low-carb diet, most people see a significant drop in high blood pressure—often within just a few days. Because of this, it may be necessary to reduce or even stop hypertension medications quickly and decisively. If not, you risk low blood pressure, dizziness, and fainting. Many patients also find that increasing their salt intake helps.
For most people, a low-carb diet combined with light cardio—such as jogging, swimming, or brisk walking—helps keep blood pressure below 140/90 mmHg. At this level, blood pressure medications are usually unnecessary and may cause more harm than good.
However, for a small percentage of people, switching to a low-carb diet does not lower their high blood pressure. It is a warning sign. It means you may have a severe and dangerous underlying condition. In this case, you should urgently seek knowledgeable doctors and consult them promptly. I plan to publish a detailed article on this issue later.
Viral and Bacterial Infections
When the body fights viral or bacterial infections, insulin sensitivity drops significantly. Science has yet to explain why, but this effect is well-known. During active infections, people with diabetes often have to increase their insulin doses. Their elevated blood sugar readings indicate this need.
Sometimes, attentive diabetics notice an unexpected rise in blood sugar with no apparent cause. Later, it turns out the reason was a hidden infection. A day or two later, symptoms of a cold, food poisoning, or another infectious illness appear. It is a good reminder of the importance of utilizing a continuous glucose monitoring (CGM) system. CGM helps detect such changes early and respond promptly, reducing the risk of serious troubles. You can read more about blood sugar monitoring here.
During infectious illnesses, insulin sensitivity drops, and people with diabetes often need higher doses of this hormone. Even if your diabetes is mild and you usually manage without daily insulin injections, it may be wise to temporarily start taking shots of long-acting insulin while you are sick. It can help stabilize your blood sugar until you recover. Ignoring this advice could permanently worsen your diabetes. This risk is not worth taking.
If you haven’t already, learn how to inject insulin right now. Buy a bottle of saline solution (your pharmacist will know what to give you) and a couple of insulin syringes. Practice the injection technique and see for yourself that it’s virtually painless. Then, make sure you always have long-acting insulin on hand, just in case.
Hormonal Imbalances
Hormonal imbalances often reduce insulin sensitivity. The most common culprits include:
- Thyroid hormones
- Cortisol, the stress hormone
- Sex hormones
- Growth hormone
Let’s look at how each of these affects insulin sensitivity—and what you can do about it.
Thyroid Hormones
The main thyroid hormones are:
- Thyroid-stimulating hormone (TSH)
- T4 (thyroxine)
- T3 (triiodothyronine)
A deficiency of thyroid hormones is called hypothyroidism, and it’s a common cause of insulin resistance.
An excess of these hormones is known as hyperthyroidism. In this case, insulin sensitivity may increase or decrease—it varies from person to person.
Treating thyroid disorders is a complex subject that goes beyond the scope of this article. If you have been diagnosed with these diseases, the carnivore diet may be worth exploring as a potential support strategy.
The Stress Hormone Cortisol
Cortisol, our primary stress hormone, is a powerful counter-insulin hormone. It blocks the action of insulin and raises blood sugar. The adrenal glands produce it.
Cortisol levels naturally peak in the dawn hours. This surge often causes blood sugar to rise early in the morning, making it harder to keep glucose levels in check before and after breakfast.
Chronic stress and lack of sleep can disrupt the conventional daily pattern of cortisol secretion. Instead of a sharp morning peak, cortisol levels become more consistent throughout the day.
This imbalance, sometimes called adrenal fatigue, is not a good sign. When it happens, people with diabetes often struggle to control their blood sugar. However, the root cause is usually the ongoing stress and not necessarily elevated cortisol levels.
Cushing’s syndrome is an endocrine disorder where the adrenal glands produce excessive cortisol. It is a rare and serious condition. People with Cushing’s syndrome experience reduced insulin sensitivity, but this is only one of many challenges they face. Often, surgical treatment is necessary to manage the syndrome.
Sex Hormones
The primary sex hormone in men is testosterone. In women, it is estrogen. Both hormones help improve insulin sensitivity. As people age, levels of these hormones naturally decline, which often leads to increased insulin resistance. This decline is a common factor contributing to the development of type 2 diabetes in middle-aged and older adults.
People motivated to live long and maintain good health should counteract the age-related decline in sex hormones by following a low-carb diet and staying physically active.
I don’t yet have a firm opinion on hormone replacement therapy. Although testosterone replacement in men shows promising effectiveness, I worry it might negatively impact life expectancy.
Growth Hormone
Growth hormone reduces insulin sensitivity. During adolescence, blood levels of this hormone fluctuate significantly, making diabetes control more challenging. These levels stabilize once the rapid growth phase ends. The key is to prevent chronic diabetes complications from developing in teenagers during this critical period.
Acromegaly is a condition caused by excess growth hormone in the blood, usually due to a small benign brain tumor. Treatment typically involves surgery and sometimes radiation or medication. Early detection, diagnosis, and treatment are necessary for better outcomes.
Genetic Predisposition Towards Insulin Resistance
Genetic predisposition to insulin resistance often shows up as an irresistible craving for carbohydrates—such as flour products, potatoes, and sweet fruits and vegetables. Our body converts most of the carbohydrates consumed into fat. After that, it stores the fat as a long-term energy reserve. The more fat reserves you have, the lower your insulin sensitivity becomes.
It is crucial to comprehend that our fat reserves originate from the carbohydrates we consume, not the fats we eat. The vegetable and animal fats in our diet are primarily burned by the body for energy rather than stored as fat. For more details, see the articles on glucose and fructose.
A genetic predisposition to insulin resistance was very advantageous for our ancestors, who often faced periods of famine. Those who gorged on carbohydrates and stored large amounts of fat during food abundance were more likely to survive the famine. The others often died without leaving offspring.
However, our living conditions today differ from those of our ancestors. For us, a genetic predisposition to insulin resistance and obesity is a problem rather than an evolutionary advantage. To counteract the adverse effects of your heredity, follow a low-carb diet and engage regularly in cardio training and weight lifting.
Age
Regarding the connection between age and insulin sensitivity, keep these points in mind:
- Children usually have very high insulin sensitivity.
- Early adolescence brings hormonal surges that cause insulin sensitivity to fluctuate.
- In middle and old age, insulin sensitivity declines gradually due to decreasing sex hormone levels.
In pre-teens, insulin sensitivity is usually very high. Parents of young children with diabetes may need to dilute insulin to avoid overdosing and causing hypoglycemia. Naturally, this applies only to children who are not obese, as obesity lowers insulin sensitivity.
In early adolescence, insulin sensitivity may decrease. Teens often find it harder to maintain tight diabetes control because their growth hormone and sex hormone levels fluctuate wildly. After puberty, hormone levels stabilize, making diabetes easier to manage.
In middle and old age, insulin sensitivity gradually declines due to a drop in sex hormone levels—testosterone in men and estrogen in women. Muscle mass may also decrease. If you want to live long and stay strong, offset it by following a low-carb diet and exercising regularly. As for hormone replacement therapy, I don’t have a clear opinion on whether it’s worth it yet.
Time of Day
You need to learn how your blood sugar usually changes throughout the day. Track it carefully for several days or weeks. Then, create an optimal daily schedule for meals, exercise, medications, insulin injections, and other activities. Coping with this task is crucial for good diabetes management. Utilizing a continuous glucose monitoring system will make your life much easier. You can read more about proper blood sugar monitoring in diabetes here.
Most diabetics struggle the most with keeping their blood sugar within normal range in the morning hours. Around 4 or 5 a.m., the body starts releasing plenty of stress hormone cortisol into the blood to help you wake up. Cortisol reduces insulin sensitivity, which can make blood sugar control more difficult at this time of the day.
Keep in mind that not all people with diabetes experience their highest blood sugar in the morning on an empty stomach or after breakfast. You might have reduced insulin sensitivity at lunch or after dinner instead. Careful blood sugar monitoring will help you identify your pattern. Use this information to adjust your diabetes management accordingly.
Personalized Diabetes Treatment
In most cases, doctors tend to prescribe nearly identical treatment plans for all their patients with diabetes. This approach allows them to minimize the time spent on each case. It’s part of a broader effort to streamline the healthcare system and reduce costs for government budgets and private insurance providers.
When prescribing standardized diabetes treatments, doctors typically ignore how an individual’s blood sugar fluctuates throughout the day. It’s up to patients to track these changes and adjust their diabetes management accordingly. It requires strong motivation to stay healthy and live a long life, along with above-average numeracy skills.
You can ask your endocrinologist for help developing and adjusting a personalized diabetes treatment plan. Good luck with it! Realistically, the best chance of creating an effective individualized plan is by carefully studying the materials provided on this website.
How the Menstrual Cycle Affects Your Insulin Sensitivity
In women, insulin sensitivity varies slightly with the menstrual cycle. Estrogen, a hormone that supports insulin action, begins to rise on the first day of menstruation and peaks around day 14.
Progesterone, a hormone that increases insulin resistance, starts rising slowly on day 14. At the same time, estrogen levels gradually decline until the end of the 28-day cycle. If pregnancy does not occur, progesterone typically peaks around day 21.
Women with type 1 diabetes often need to adjust their insulin doses slightly depending on the stage of their menstrual cycle. Those with type 2 diabetes may also notice changes in blood sugar levels and insulin needs throughout the cycle.
Weather, Air Temperature
Insulin sensitivity tends to be higher in warm weather and lower in cold weather, all other factors being equal. As temperatures drop, your insulin needs may rise slightly; as it warms up, they may decrease. It is a standard pattern and nothing to worry about.
Weather is a relatively weak factor affecting insulin sensitivity. Changes in diet, physical activity, or medication have a much stronger influence. They will overshadow any effects of weather variations. You can only notice the impact of weather on your insulin needs during rare periods when all other aspects of your lifestyle remain stable.
Alcohol Consumption
When there is a significant amount of alcohol in the body, the liver stops breaking down glycogen and releasing glucose into the blood. As a result, a standard insulin dose can have a much stronger effect and cause hypoglycemia. In other words, during moderate to severe alcohol intoxication, insulin sensitivity is significantly increased.
The danger is this: severe hypoglycemia causing loss of consciousness looks almost identical to loss of consciousness from alcohol intoxication. When someone is intoxicated, they usually don’t need help and will wake up after sleeping it off. But if the cause is severe hypoglycemia, urgent medical care is critical. Without it, the risk of death is very high.
A reliable way to tell severe hypoglycemia with loss of consciousness apart from alcohol intoxication is to measure blood sugar. However, at parties or during drinking binges, people rarely think to check the blood glucose of someone who has passed out. The bottom line is this: diabetics who use insulin injections should avoid getting drunk. When intoxicated, they face much higher risks than others.