By adopting a strict low-carbohydrate diet and optimizing their use of insulin and diabetes medications, individuals with both type 1 and type 2 diabetes can effectively regulate their blood glucose levels and maintain them within the normal range. In this context, “normal blood glucose” refers to the values typically observed in healthy individuals with normal metabolic functions. For adolescents and adults, this corresponds to approximately 83 mg/dL ±10 mg/dL, i.e., 73-93 mg/dL. Before reaching puberty, healthy children tend to have blood glucose levels about 10 mg/dL lower. Read more about it here.
For people with diabetes who have lived with chronically high blood sugar (hyperglycemia) for years, a sudden normalization of blood glucose levels—especially if done rapidly—can lead to several complications. These include:
- Hypoglycemia symptoms.
- Worsening of diabetic retinopathy.
- Potential increase in kidney problems.
- Burning, tingling, stabbing pain in the feet or hands.
Below is a closer examination of these risks and the steps you can take to avoid them. You may want to review our disclaimer before continuing.
The Alarming Prevalence of Poorly Controlled Diabetes
Across the globe, a significant population lives with type 2 and type 1 diabetes, numbering in the hundreds of millions, who unfortunately manage their condition incorrectly or with a careless approach. These folks consistently experience blood glucose levels exceeding the normal range observed in healthy individuals. This detrimental state of affairs persists for many years. Over time, their bodies have become accustomed to it.
When individuals with poorly managed diabetes transition to a low-carbohydrate diabetes control system and rapidly bring their blood sugar levels back to normal, they may encounter side effects. These side effects can vary, ranging from mild discomfort to more severe and potentially hazardous consequences, such as disability or even death. This risk becomes particularly pronounced for individuals who have endured 8-10 years or longer of improperly treated diabetes.
Below is a detailed description of the potential challenges associated with rapidly normalizing blood glucose levels. It applies to individuals with diabetes who have grown accustomed to elevated blood glucose levels over several years, usually at least 8-10 years. With proper actions, even individuals with a lengthy history of poorly managed diabetes can avoid most of these issues. However, accomplishing this feat will require significant effort.
Temporary Well-Being Decline, Fainting
For countless individuals with diabetes, living with chronically elevated blood sugar levels has become the norm, spanning many years or even decades. Their bodies have adapted to this persistent state. When these patients transition to a low-carbohydrate diabetes management system, they can effectively restore their blood glucose levels to a normal range within several days. Nevertheless, during the initial few days or weeks, their bodies may perceive this shift as hypoglycemia.
Severe hypoglycemia can have grave consequences, including loss of consciousness, permanent brain damage, and even mortality. When it comes to normalizing blood glucose levels that have been elevated for an extended period, such severe outcomes are unlikely to occur. Nonetheless, individuals with diabetes who have recently transitioned from conventional treatment practices to a genuine low-carbohydrate approach may still encounter unpleasant symptoms. These can manifest as constant hunger, irritability, dizziness, and even episodes of fainting. In summary, their overall well-being may experience a notable decline.
The only possible solution of this issue is to reduce elevated blood glucose levels to normal gradually rather than attempting a rapid normalization. It may take several weeks or even about two months. Allowing sufficient time for individuals with a lengthy history of poorly managed diabetes to adapt to a new regimen is crucial. However, it is easier said than done. Implementing a low-carbohydrate diet and making insulin dose adjustments to achieve normal blood glucose levels is not simple. Aiming for a “moderately elevated” blood glucose level adds an additional layer of complexity. To get out of the vicious cycle, diabetics must possess high motivation, continuously track and process their data.
Exacerbation of Eye Problems That May Result in Permanent Blindness
Retinopathy is a dangerous complication associated with diabetes that impacts the eyes. This condition occurs as a result of high blood glucose levels that gradually impair the delicate blood vessels responsible for nourishing the eyes. As the illness progresses, it can give rise to hemorrhaging within the eyes, the formation of visible blood clots in the eyes, retinal detachment, and eventually, even complete loss of vision.
The following warning applies to diabetics with a history of hemorrhaging within the eyes and other problems caused by diabetic retinopathy. Transitioning to a low-carbohydrate management system for your diabetes can potentially give rise to significant challenges in the initial days and weeks. During this period, there exists a heightened risk of encountering hemorrhaging and blood clots formation within the eyes, retinal detachment, and even the onset of complete blindness.
It is of utmost importance to have prompt access to an experienced ophthalmologist skilled in treating diabetic retinopathy, including surgical interventions. Ensure that you have such assistance readily available, even during nighttime emergencies. Also, try to bring your blood sugar back to normal gradually, over several weeks or even a couple of months, rather than all at once. This process may not be effortless and demand high levels of motivation and cognitive capacity.
The warnings above should not deter you from switching to a low-carb diabetes management system unless you have very advanced kidney disease (see below). While there is an increased risk of worsening diabetic retinopathy symptoms, including the possibility of total blindness, the potential benefits far outweigh these risks. To mitigate risks, establish contact with an experienced ophthalmologist who is readily accessible.
Worsening Renal Diabetes Complications, Kidney Failure
Switching to a low-carbohydrate diet carries potential risks for individuals with compromised kidney function, including patients diagnosed with kidney complications of diabetes (diabetic nephropathy). There is a concern that transitioning to a low-carbohydrate diet could potentially accelerate the progression of kidney destruction. It may lead to needing dialysis or a kidney transplant sooner. The extent of this risk is a matter of controversy. It remains a subject of ongoing debate.
The appropriateness of transitioning to a low-carbohydrate diet for individuals with diabetic nephropathy remains a highly contentious topic. Numerous doctors and health officials believe that adopting a low-carbohydrate diet can potentially accelerate kidney damage in diabetics. These specialists are especially wary of a low-carb, high-protein diet. However, this book takes a contrasting stance and recommends just such a diet, emphasizing the harmful effects of protein deficiency.
Rethinking the Kidney Risks of Low-Carb Diets
Until the 2000s, there was a consensus in medical science that low-carbohydrate diets are detrimental to individuals with diabetes. Recently, scientists have published many articles in medical journals that challenge this viewpoint. See, for example, Mitchell, N. S., Scialla, J. J., & Yancy, W. S. (2019). Are low-carbohydrate diets safe in diabetic and nondiabetic chronic kidney disease? Annals of the New York Academy of Sciences. The conclusion reached by the authors is as follows.
The notion of a low-carbohydrate diet being harmful to individuals with diabetes lacks sufficient evidence and requires further research.
You can find many other recent articles claiming the same thing.
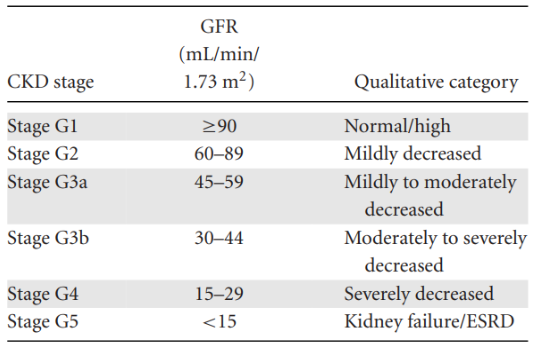
The doctors measure the severity of chronic kidney disease (CKD) by the ratio of albumin to creatinine in the urine and by the glomerular filtration rate (GFR).
The following statements represent my present belief, which is not extensively supported by objective data as none are currently available. I have formed this opinion based on scarce information from private discussions with patients and several public sources. If new data emerge in the future, my today’s belief may be proven incorrect. Such a mistake can have dire consequences for you, namely that your kidneys may suffer due to the erroneous transition to a low-carb diet.
Should You Go Low-Carb If You Have Kidney Disease?
Patients with stages G1 and G2 of chronic kidney disease can transition to a low-carbohydrate diet safely without posing a risk to their kidney health. In stage G3a, it is also likely safe to make the switch. In stage G3b, I would still switch to the low-carbohydrate diabetes control system as the risk-benefit ratio appears favorable. At this stage of chronic kidney disease, continuing with a standard diet and traditional diabetes management methods will likely result quickly in disability and death. Regarding stages 4 and 5 of chronic kidney disease, probably, it is too late to opt for a low-carbohydrate diabetes control system.
In addition to adopting a low-carbohydrate diet, adhering to the other recommendations outlined in this book is essential. It includes carefully considering the intricacies of insulin usage and diabetes medications, as detailed in the following chapters.
The ultimate objective is to achieve stable and healthy blood glucose levels. You can accomplish it only by embracing a low-carbohydrate diet. In addition to the diet, it is crucial to determine optimal insulin doses and establish an appropriate injection schedule. Also, be attentive to medications prescribed for diabetes, hypertension, and other relevant conditions. In short, do whatever it takes to achieve and sustain normal blood sugars, namely, 83 mg/dL ±10 mg/dL around the clock. Otherwise, you can damage your kidneys and other vital organs.
In the event of a change in my perspective regarding the impact of a low-carbohydrate diet on kidney health in diabetes, I am committed to promptly communicating this update through various channels, including my email newsletter, social networks, and future editions of this book. However, I cannot undo any harm already incurred due to previous erroneous recommendations.
Burning, Tingling, or Stabbing Pain in the Feet or Hands
Your muscles move because your nerves send them signals. When you have diabetes, high blood sugar can damage those nerves. This kind of damage is called diabetic neuropathy, and it occurs pretty often. Like most long-term complications of diabetes, it happens when your blood sugar stays elevated for too long.
The most common sign of diabetic neuropathy is losing sensitivity in your arms and legs — to touch, pain, temperature, and more. Because of this, millions of people with diabetes don’t notice when their feet get injured, burned, or frostbitten. These unnoticed wounds can get worse over time, sometimes to the point where amputation is the only option.
Once your blood sugar stays consistently normal for a few days, your damaged nerve fibers can start to heal. As the feeling returns, some people go through a difficult phase — they feel intense pain in their legs or arms. It happens because the nerves are waking back up. The pain usually fades after a month or two once the nerves finish healing from diabetic neuropathy.
As far as I know, no medication can fix this kind of pain. Some drugs might dull it, but these powerful drugs usually come with serious side effects. It is better to tough the pain out. Try to remind yourself that this pain is a sign your body is healing from a dangerous complication of diabetes.
Don’t confuse the pain that comes during nerve healing with the pain caused by ongoing high blood sugar. As I mentioned earlier, diabetic neuropathy usually leads to numbness in the limbs. But for some people, it causes intense pain instead of loss of sensation. This kind of pain is brutal — and most painkillers don’t help much.
The severe pain from worsening diabetic neuropathy often pushes people to finally take their diabetes seriously because nothing except normalizing blood sugar can relieve their suffering. In that sense, the pain is better than the numbness. At least it forces action. Of course, if you’re going through that kind of hell right now, you probably won’t agree.
Strategies to Mitigate These Challenges
The cautions outlined above pertain mostly to individuals who have experienced long-term mismanagement of diabetes. Their bodies have become accustomed to chronically elevated blood sugar levels. It can lead to misinterpretation of normal blood glucose levels as hypoglycemia. Additionally, these patients may have developed diabetes complications in their eyes and kidneys. These complications may worsen during the initial days and weeks after transitioning to a low-carb system for managing impaired glucose metabolism.
Before transitioning to a low-carb diabetes management approach, it is recommended that you:
- Undergo blood and urine tests in a laboratory to assess kidney function.
- Seek advice from an experienced ophthalmologist who specializes in diabetic retinopathy.
- Familiarize yourself with the symptoms and treatments for hypoglycemia (low blood sugar).
To gradually bring your blood sugar back to normal, it is advisable to make adjustments over several weeks or even 1-2 months. You can achieve it by experimenting with the amount of carbohydrates consumed, adjusting doses of insulin and diabetes medications, and incorporating exercise into your routine. As a general rule, it is better to eliminate all the illicit foods high in carbohydrates right away. After that, to regulate your blood glucose levels, experiment with insulin and diabetes medication dosages.
To gradually normalize your blood glucose levels, it is necessary to monitor them frequently. After every measurement, make slight adjustments to your insulin and medication doses. This process demands a high level of motivation and cognitive ability. As of today, I am not aware of any easier yet effective alternative for managing diabetes. Simplistic approaches to diabetes treatment inevitably result in complications, disability, and reduced life expectancy among patients.
Prepare Ahead: Resources That Will Support You
I highly recommend acquiring and utilizing a continuous glucose monitoring system to simplify your life and improve your chances of success. It is essential to prioritize investing in this device and its supplies. Additionally, it is beneficial to seek out an endocrinologist who supports a low-carbohydrate diet for diabetes and establish a relationship with them. While it would be fortunate to find such an endocrinologist, it is not mandatory.
Switching to a low-carb diet can cause weakness and dizziness in the first few days. These symptoms can affect not only those with diabetes but also individuals without the condition. To improve your well-being, increase the intake of fluid and salt. Consuming salted meat, chicken, or fish broth can be especially helpful in alleviating the issues.
Along with broths, include herbal teas in your diet. Ensure that teas are free from sugar, honey, other carbohydrates, and excessive amounts of caffeine or other stimulants. In general, when transitioning to a low-carbohydrate, high-protein diet, it is advisable to consume an ample amount of fluids.
Avoid having concentrated, dark-colored urine. Stay hydrated by drinking plenty of fluids to ensure your urine remains diluted and nearly transparent. Enhancing hydration is a relatively unknown, straightforward, and remarkably effective way to boost your physical and mental well-being.