For both adults and children with diabetes, insulin pumps tend to cause more problems than they solve. The same applies to newer systems that combine a pump with a continuous glucose monitor. These devices automate insulin dosing and delivery, but the added complexity often creates more risks than benefits. Even if cost isn’t an issue, utilizing an insulin pump is usually not a good idea.
A better option is traditional insulin injections, either with insulin pens or even good old syringes. Below, you’ll find a detailed explanation of why this approach is safer and more effective for most people with diabetes.
Start by reading the introduction to insulin pumps here. It will help you understand:
- What components make up these devices
- How they function
- The differences between tubed and tubeless models
That article highlights the potential benefits of insulin pumps. But below, we take a closer look at their downsides—disadvantages that, in most cases, outweigh the advantages.
First, learn the basics of the low-carb diabetes management system here. It offers a strong alternative to using an insulin pump. This approach works well for both type 1 and type 2 diabetes in adults and children. It helps keep healthy blood sugar levels without the typical wide swings. The result is better overall health and the most reliable protection against diabetes-related complications.
It’s best to avoid using an insulin pump. However, a continuous glucose monitoring (CGM) system is strongly recommended. The sensors used with CGMs aren’t cheap, but they’re not prohibitively expensive either. Do whatever you can to make room in your budget for them. Using a CGM can greatly improve your blood sugar control and significantly reduce the risk of long-term diabetes complications. You can read more aboutthe proper blood glucose monitoring here.
Insulin Pump Therapy: What You Pay Beyond the Device
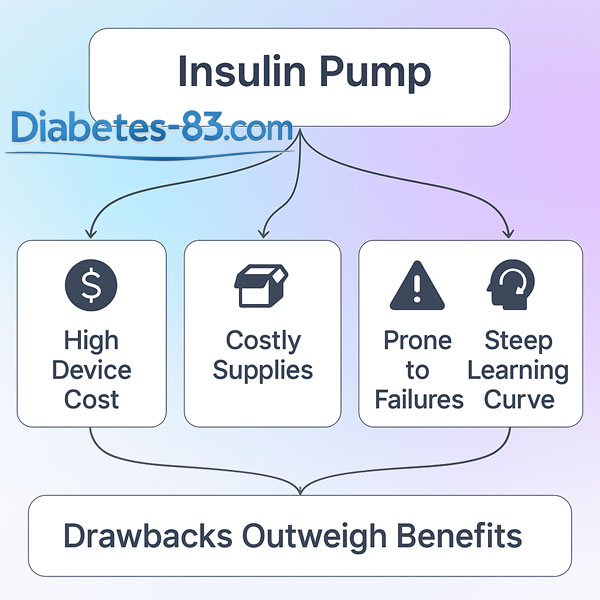
An insulin pump is a costly device. The latest models that calculate insulin doses every few minutes and deliver them automatically are often outrageously pricey. These integrated systems are marketed as fully automated. However, despite their high price, they fall short in key areas. Their insulin dose calculations often lack the accuracy for safe and effective treatment. Reliability is also a serious concern. These devices do not perform well enough to justify their cost.
Besides the high upfront cost of buying an insulin pump, you also need to budget for ongoing expenses, including:
- Infusion sets, which consist of a tube and a cannula
- Reservoirs that hold insulin inside the pump
- Replaceable batteries or rechargeable accumulators
- Rapid-acting insulin to fill the reservoirs
- Various small supplies like bandages, wet wipes, and more
These regular costs add up quickly and should factor into your decision before choosing an insulin pump.
You’ll have to change infusion sets and insulin reservoirs every 2 to 3 days. It prevents bacterial growth and the formation of insulin crystals. Pump manufacturers work hard to stop users from using cheaper supplies with their devices. Most likely, you’ll have to buy expensive branded infusion sets and reservoirs. These will cost you around $100 to $200 per month. For insulin pump companies, selling supplies brings in as much revenue as selling the devices.
Sometimes, people with diabetes get the government or their insurance to cover the cost of insulin pumps and supplies. But often, this support is not available. In those cases, adults with diabetes and parents of diabetic children have to pay all expenses themselves.
If you can’t afford an insulin pump, your only option is to inject insulin using syringes or insulin pens. In that case, you don’t need to worry about the downsides of insulin pumps. But if you have enough money for these expensive devices, it’s worth reading this page all the way through.
Frequent Failures Caused by Unreliable Systems
Insulin pumps are fragile and unreliable because of their complexity. Simplifying them and making them more dependable isn’t possible right now, and it is unlikely to happen in the next few years without major, unexpected technological breakthroughs. I don’t see any signs that such breakthroughs are coming soon.
People with diabetes who use insulin pumps face frequent malfunctions. The most common problems include:
- The plastic tube bends, blocking insulin delivery
- The patch peels off, often because of sweat, preventing insulin from reaching under the skin
- Skin irritation, infections, and scarring where the cannula is inserted
- Insulin crystals form and clog the channel
- Insulin leaks
- The battery runs out of charge
- The pump’s motor breaks, stopping insulin delivery
- Communication from the continuous glucose monitor fails, disrupting automatic insulin dosing
- Software glitches
- Various types of human errors, which we will discuss in detail below
These and other issues make insulin pumps challenging to use.
The Burden of Wearing a Device 24/7
Sometimes, you might not want to reveal that you have diabetes. But if you forget to remove your insulin pump, it can easily give you away.
Here are some other common challenges users face:
- Sleeping with an insulin pump can be uncomfortable and hard to get used to.
- Many people with diabetes say it causes psychological problems during sex.
- You can’t do many sports while wearing the pump.
- Airport security may stop you for questions when you board a plane.
These everyday situations can make using an insulin pump inconvenient and stressful.
Many manufacturers claim their insulin pumps are waterproof, meaning you can shower or swim while wearing them. However, these claims don’t always inspire confidence. It is safer to remove the pump before any water activities. Afterward, carefully put it back on.
It’s important to stress that insulin pens or syringes users don’t face any problems listed in this section or the previous one.
The Steep Learning Curve
Many adults with diabetes and parents of diabetic children believe that mastering and using an insulin pump is easier than injecting insulin with syringes or pens. However, this is a misconception.
Be ready to invest a lot of time and effort in learning the nuances of your insulin pump. This is true even for the latest models that automatically calculate insulin doses. Older models, lacking this feature, require even more skill and attention.
You’ll need to learn how to use the insulin pump’s complex interface to program it correctly. It may turn out to be a challenging and complex task. On top of that, you’ll have to master several hands-on assignments, including:
- Inserting and securing infusion sets
- Replacing reservoirs and filling them with insulin
- Keeping track of battery levels
- Identifying and fixing dozens of possible issues that may come up
Using an insulin pump isn’t just plug-and-play—it requires technical and analytical skills, attention to detail, and constant monitoring.
Many people buy an insulin pump, hoping it will ease the mental burden of managing diabetes. But that hope is unrealistic. Just like anyone else with diabetes, you’ll still need to understand how insulin works and how to calculate the correct doses. You must learn how insulin needs change based on the amount of carbohydrates you eat and many other factors that affect insulin sensitivity.
The pump can help deliver insulin. However, it can’t replace the knowledge and judgment needed for effective diabetes management.
Common Mistakes When Using an Insulin Pump
Using an insulin pump is complex, and mistakes are common. Here are some of the most frequent ones:
- Programming errors caused by a poor understanding of how insulin works
- Incorrect insulin dosing due to miscounting carbohydrate intake
- Programming mistakes made out of inattention
- Forgetting to put the pump back on after temporarily removing it
- Inserting the needle into the skin at the wrong angle or depth
- Failing to secure the cannula to the skin properly
- Forgetting to rotate injection sites leads to skin damage
- Not removing air bubbles from the insulin
- Overlooking a blockage that prevents insulin from flowing through the tube
- Placing the cannula on irritated or inflamed skin
- Ignoring warning signals from the pump
- Not bringing enough supplies when traveling
- Neglecting to check the accuracy of the continuous glucose monitoring regularly
- Failing to replace infusion sets, reservoirs, or other supplies on time
Technical failures of insulin pumps are common due to their complexity and unreliability. Also, human errors happen often. Together, these issues can leave a person with diabetes without the insulin they need for a few hours and sometimes for an entire day or more.
When the body doesn’t get enough insulin, blood sugar stays high. Over time, it leads to the development of chronic diabetes complications. These can affect the legs, eyes, kidneys, immune system, and many other parts of the body.
In people with type 1 diabetes, a pump failure can also trigger a serious and potentially life-threatening condition called diabetic ketoacidosis (DKA). It may happen quickly and require urgent medical attention.
Diabetic Ketoacidosis
Diabetic ketoacidosis is a serious, fast-developing, and potentially life-threatening complication of type 1 diabetes. It can occur when the body doesn’t have enough insulin. One common cause is a disruption in insulin delivery—sometimes due to problems with the insulin pump. Prompt recognition and treatment are critical to prevent severe outcomes.
Mechanism
When insulin levels in the blood drop, the body switches to burning fat for energy. It is a perfectly natural process that yields substances called ketones. For overweight people with type 2 diabetes, this is just what they need and want.
However, in the complete absence of insulin, especially in people with type 1 diabetes, this process goes out of control. Ketone levels rise rapidly, making the blood dangerously acidic. It is the core of diabetic ketoacidosis. This severe and potentially deadly condition requires immediate treatment.
Symptoms
Symptoms of diabetic ketoacidosis:
- Blood sugar is high—at least 160 mg/dL, and often 220–260 mg/dL or more
- Urine test strips show the presence of ketones and maybe also glucose
- Possible symptoms include fatigue, dizziness, nausea, vomiting, and confusion—but these may be completely absent
- The person may have a noticeable smell of acetone on their breath, though this isn’t always present
Somebody should recognize the warning signs and take action quickly. Otherwise, the condition can progress to the loss of consciousness and even death.
Basal Insulin Level
Normally, the body maintains a modest, steady level of insulin in the blood 24 hours a day to prevent diabetic ketoacidosis. It is called the basal insulin level. People with diabetes usually get it through injections of long-acting insulin, which works for at least 12 hours.
However, insulin pumps deliver only fast-acting insulin that lasts no more than a few hours. That means if the pump malfunctions or stops working, insulin levels in the blood can drop to zero within 4 to 6 hours. In this situation, patients face a serious risk of losing consciousness or even dying.
Prevention
Preventing the diabetic ketoacidosis:
- The simplest way to avoid risks is to stop using an insulin pump altogether and switch to basal-bolus insulin therapy.
- If you adhere to the pump, prepare well by learning to recognize and troubleshoot common problems.
- Ensure your pump sounds audible alarms for low insulin, low battery, or blocked insulin delivery.
- Keep a fast-acting insulin pen handy in case the pump fails.
- Always know the emergency phone number for quick help.
Conclusion
I hope the information on this page has convinced you that using an insulin pump is not advisable. Avoid it—even if you can easily afford one. Instead, choose insulin injections with traditional syringes or pens.
I often emphasize that managing diabetes well demands strong motivation and above-average cognitive skills. Read more about it here. Unfortunately, an insulin pump cannot replace these essential traits. Without them, this expensive electronic device is more likely to cause harm than provide benefits.