Sulfonylurea derivatives are a group of drugs used to treat type 2 diabetes. Common examples include glibenclamide (Glyburide), glipizide (Glucotrol, Minodiab), gliclazide (Diamicron, Diaprel), and glimepiride (Amaryl). These medications are popular among both patients and doctors. However, their drawbacks often outweigh their benefits.
If you want to live a long life, it’s best to avoid taking sulfonylurea derivatives. A low-carb approach to managing diabetes offers a safer and more effective alternative.
This page covers the following topics in detail:
- Which drugs belong to the sulfonylurea derivatives group
- How they work to lower blood sugar
- Why many people with type 2 diabetes—and their doctors—prefer these medications
- Why you should avoid them, even though they may seem beneficial at first glance
In short, sulfonylureas effectively lower blood sugar in people with newly diagnosed type 2 diabetes. However, they likely don’t extend life expectancy—and may even shorten it. The reasons behind this are explained in detail below.
In diabetes, lowering blood sugar doesn’t automatically lead to a longer life. The method used to reduce blood glucose plays a crucial role. It is a key idea that not many doctors—and even fewer patients—fully understand.
Sulfonylurea Derivatives: List of Drugs
The first sulfonylurea drugs for diabetes appeared in the 1950s. They often triggered severe hypoglycemia, and in some cases, this led to death. These early medications are no longer used. The second generation drugs have replaced them, offering a milder and safer reduction in blood sugar.
| Generic Name | Trade Name(s) | |
|---|---|---|
| Glibenclamide | Glyburide, Daonil, Euglucon | Once or twice daily |
| Glipizide | Glucotrol, Minodiab | Once or twice daily |
| Gliclazide | Diamicron, Diaprel | Once daily (MR) |
| Glimepiride | Amaryl | Once daily |
The drugs listed above differ in their potency, duration of action, risk of hypoglycemia, and suitability for specific patient populations.
Glibenclamide (Glyburide)
Glibenclamide (Glyburide) is a highly potent drug with a long half-life and strong glucose-lowering effect. However, it has a high risk of causing prolonged and severe hypoglycemia, particularly in older adults or those with impaired renal function. Due to these safety concerns, it is less commonly prescribed in developed countries today.
Glipizide (Glucotrol, Minodiab)
Glipizide (Glucotrol, Minodiab) has a shorter half-life than glibenclamide and a more moderate risk of hypoglycemia. People with type 2 diabetes typically take it once or twice daily. Doctors consider it safer in elderly patients or those with mild kidney impairment. Its relatively short duration of action makes it a flexible option in some treatment plans.
Gliclazide (Diamicron, Diaprel)
Gliclazide (Diamicron, Diaprel) is known for its favorable safety profile, with a lower incidence of hypoglycemia compared to other sulfonylurea derivatives. The modified-release (MR) formulation allows once-daily dosing and provides steady blood sugar control throughout the day. It may also have mild antioxidant properties and better cardiovascular safety, making it a preferred sulfonylurea in several international guidelines.
Glimepiride (Amaryl)
Glimepiride (Amaryl) is one of the most widely used modern sulfonylureas. It is administered once daily and has a relatively low risk of hypoglycemia if patients do not exceed the recommended dose and eat on time. Like the other drugs discussed here, it causes the beta cells of the pancreas to release more insulin into the blood. Some studies suggest that it may also exert insulin-sensitizing effects in peripheral tissues.
Mechanism of Action
In the human body, beta cells in the pancreas produce insulin. Sulfonylurea drugs stimulate these beta cells to release more insulin into the bloodstream. The insulin then lowers blood sugar levels.
Normally, beta cells release insulin only when blood glucose levels are high. However, sulfonylurea derivatives cause these cells to release insulin regardless of blood sugar levels. When insulin is high but glucose is low, hypoglycemia can occur. It is a common side effect of the drugs discussed here.
Why Sulfonylurea Derivatives Are Popular
People with diabetes and their doctors favor sulfonylurea derivatives for several reasons. Patients appreciate these drugs because:
- They are easy to use.
- They are affordable.
- They create the illusion of effective treatment.
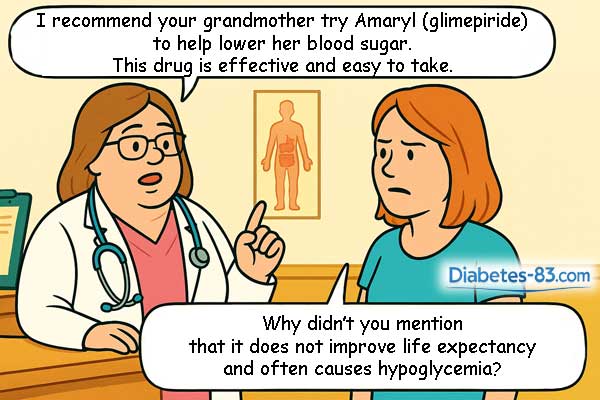
Doctors favor sulfonylurea drugs because they can prescribe them quickly and send patients home with minimal time per visit. Patients usually accept these pills willingly and don’t ask many questions. Compared to insulin, this ease makes sulfonylureas a convenient choice for doctors.
Sulfonylurea derivatives come in tablet form and are taken once or twice daily with meals. Unlike insulin, they don’t require injections. When taking these drugs, patients usually don’t have to follow a strict diet. Both doctors and drug instructions often overlook nutrition, assuming that diabetics can safely eat whatever they want.
Most sulfonylureas that are popular today have been available since the 1970s. These are old drugs whose patents have expired long ago. Multiple pharmaceutical companies produce them, creating competition. As a result, these pills are more affordable than newer diabetes medications.
In the first years of use, sulfonylurea derivatives create the illusion of effective treatment for people with type 2 diabetes. While taking these drugs, glucose meters or continuous glucose monitors usually show a significant drop in blood sugar. Patients don’t need to follow a strict diet to see these results. Moreover, trying a low-carbohydrate diet while on sulfonylureas can increase the risk of hypoglycemia.
Why These Drugs Are a Trap for Diabetes Patients
Sulfonylurea derivative drugs are a trap for people with type 2 diabetes. Although these pills lower blood sugar and glycated hemoglobin, they do not extend life expectancy. In contrast, alternative low-carb diabetes treatment can add 10 to 30 years to your life while keeping your body and mind healthy. You can achieve great results without having to suffer from constant hunger. You also won’t need to push yourself too hard during workouts.
Sulfonylurea derivatives harm the body by negatively affecting metabolism over time. Here’s how they cause damage:
- They reduce insulin sensitivity and promote weight gain.
- Increased obesity raises blood pressure.
- High blood pressure, combined with obesity and diabetes, increases the risk of early death from heart attack or stroke.
- These drugs also carry the risk of severe hypoglycemia, which can be fatal.
- Over time, they destroy beta cells, causing the body to stop producing insulin.
If you have type 2 diabetes and want to live a long life, you should focus on improving your insulin sensitivity. However, taking sulfonylurea tablets lowers insulin sensitivity. It often leads to weight gain and makes it difficult to control high blood pressure. In this situation, early death from a heart attack or stroke becomes very likely. Learn more about insulin sensitivity—how to boost and maintain it high—here.
Pancreatic Beta Cells Depletion
In type 2 diabetes, patients usually have low insulin sensitivity. The body needs abnormally large amounts of this hormone to keep blood sugar near normal. This demand puts a strain on the pancreatic beta cells, which struggle to keep up.
Using sulfonylurea drugs to stimulate these exhausted cells is like forcing a tired horse to pull a heavy cart uphill. If the owner is careless and harsh, the horse will eventually die. Similarly, sulfonylurea drugs can cause beta cells to die off.
When this happens, the body stops producing insulin, and patients must rely on injections. In reality, this outcome is rare because most patients die from heart attacks or strokes before most of their beta cells pass out.
Impact on Life Expectancy
I’ve searched but haven’t found a single article claiming that sulfonylurea derivatives increase life expectancy in people with diabetes. And I am unlikely to discover such papers someday later. Once the patents expire, there remains little financial incentive for researchers to keep studying the old drugs.
Another concern is how sulfonylurea derivatives affect the risk of heart attack and stroke. The early drugs from the 1950s, including Tolbutamide, Chlorpropamide, Acetohexamide, and Tolazamide, clearly increased this risk. As for the newer versions, experts often claim they are safer. They rely on statistical tricks to create that impression. Glibenclamide, glipizide, gliclazide, and glimepiride probably do not reduce the risk of heart attack or stroke.
It is instructive and amusing to see how medical journals, textbooks, and reference guides avoid discussing the impact of sulfonylurea derivatives on life expectancy. The same pattern shows up with many other widely used drugs for chronic conditions—statins for cholesterol, for example.
In each case, patients are led to believe that better lab results mean they’ll live longer. For sulfonylureas, it’s lower blood glucose; for statins, it’s lower cholesterol. But improved numbers don’t always translate into longer or healthier lives. Unfortunately, doctors and researchers rarely take the time to correct these mistaken assumptions.